
In just five months, a nonliving particle one hundredth the diameter of a human hair has claimed the lives of more U.S. citizens than the Vietnam and Korean wars combined. This particle is, of course, the novel coronavirus known as COVID-19. Can scientists and medical professionals find a way to stop it before it reaps further destruction?
With the ability to switch from a nonliving to a living state after hijacking a host cell’s replication machinery, viruses are intricate rogue proteins that occupy a mysterious realm between biochemistry and quantum mechanics. You cannot “kill” viruses as they are not even alive in the first place, and the field of biochemistry is currently not advanced enough to annihilate all of these sub-microscopic parasites outright without harming you, too. However, viruses utilize a variety of chemicals to accomplish their replication cycles, and it is these specific chemicals that are vulnerable to attack.
Possible treatments for viruses are classified into one of two groups: drugs that inhibit viral replication and drugs that modify your immune response.
To understand how antiviral drugs work, you must know the substances involved in viral replication. COVID-19, aka SARS-CoV-2 (severe acute respiratory system coronavirus 2), is a single-stranded RNA virus that enters your cells by binding to a specific receptor on their surfaces, triggering endocytosis (cell entry). The virus reverse transcribes its RNA into double-stranded DNA, the blueprint for protein synthesis, using an enzyme called RNA polymerase. This enzyme lacks a proofreading function, so the resulting DNA code will mutate over time. When COVID-19’s completed DNA is integrated into your cell’s genome, your cell exhausts its own resources manufacturing more viruses.
The viruses escape and infect other cells, eventually killing them.
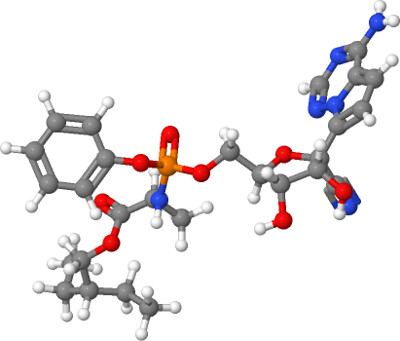
Remdesivir is the most promising antiviral drug to date, and is the only one authorized by the U.S. Food and Drug Administration for emergency use. Its molecular structure mimics that of adenine, a nucleic acid in DNA. When the viruses’ RNA polymerase mistakenly adds a Remdesivir molecule in place of adenine, the reverse transcription process is stopped. The drug’s developer, Gilead, applied for FDA approval Aug. 10 for regular use after presenting preliminary evidence proving the drug’s effectiveness. Remdesivir is not a cure for COVID-19; according to the study, treatment only reduces the recovery time of infected patients and does not protect against death. FDA approval is currently pending.
Why prioritize usage of drugs when you could just prevent people from contracting COVID-19 in the first place?
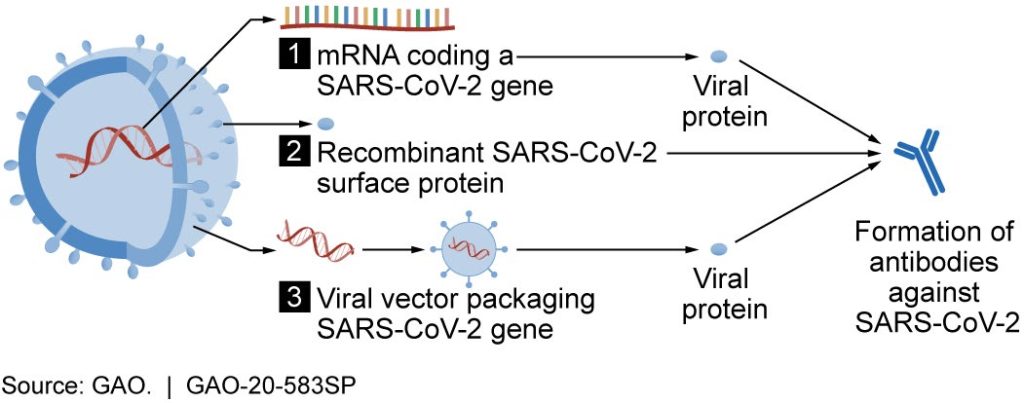
This is where drugs that modify your immune response – vaccines – come into play. Vaccination is the best way to drastically reduce COVID-19 transmission and to grant immunity to the general public. Antibodies are protective proteins naturally synthesized by your body whenever antigens (foreign substances) invade it. By introducing a weakened form of the virus or a portion of the viruses’ protein structure into your body, vaccines train your immune system to manufacture its own antibodies in a phenomenon known as active immunity. When you are infected with the actual virus, your immune system swiftly identifies the pathogen’s protein pattern, induces apoptosis (cell death) in all affected cells, and stops viral spread in its tracks.
Unfortunately, vaccine development is a long and arduous process often riddled with complications, and rushing the development process can sacrifice drug effectiveness and even trigger dangerous immune reactions in patients. To be deemed safe and effective, immunological response data from thousands of testing subjects from specific populations (especially those with underlying health issues and senior citizens) must be compiled and analyzed. This procedure alone can take months or even years. After a vaccine is considered safe and effective, there is the additional hurdle of manufacturing and distributing the vaccine to the entire population.
The rate of vaccine development is progressing at historically fast speeds. According to Johns Hopkins Coronavirus Resource Center, the first COVID-19 vaccine was developed for testing just six weeks after the viral sequence was decoded. In comparison, the vaccine for Influenza – another RNA virus infecting the respiratory system – took 20 years to be developed and 26 years to be approved. In fact, by the time regular citizens were inoculated with this flu vaccine, it was ineffective because the virus had mutated by then.
The most promising SARS-CoV-2 vaccine, Moderna, entered its final phase of testing among 30,000 patients on July 27. Dr. Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases, has predicted that researchers will be able to determine Moderna’s effectiveness by November or December this year, perhaps sooner. The vaccine does its job by transmitting mRNA (messenger RNA) molecules transcribed from DNA to your cell’s genomes, which causes them to assemble portions of COVID-19 proteins. By introducing these inactive foreign proteins into your body, the vaccine compels your immune system to manufacture antibodies that will identify and eliminate the actual virus. The introduction of a vaccine to the American public would finally allow our country to regain some semblance of normalcy.
and Analytics
The way each person responds to SARS-CoV-2 infection depends on individual genetics, age and pre-existing health conditions. Some patients are not even aware of infection, while others exhibit life-threatening symptoms. COVID-19 enters cells by binding a receptor called the angiotensin enzyme converting 2 (ACE2) receptor. Angiotensin 2 is a powerful enzyme that causes your blood pressure levels to skyrocket and is implicated in inflammation in a way that is still not fully understood. For some, SARS-CoV-2 wreaks havoc on the cardiovascular system, which then damages vascularized organs requiring a constant blood supply. Despite having a 3-4% mortality rate, evidence suggests that COVID-19 is capable of inflicting lasting damage on highly vascularized organs including the lungs and brain.
Scientific advancement is not based on a couple of scientific studies or published papers. Instead, it is founded upon decades of research. Medical professionals, scientists and governments across the globe are engaged in a race unlike any other in history to develop a safe and effective vaccine, and we have learned about COVID-19 faster than any infectious disease in history.
Unanswered questions, however maddening they may be, are powerful catalysts for scientific advancement. As we expand the breadth and depth of our knowledge, not only will we have more answers, but we will have a better understanding of the right questions to ask. To quote Douglas Adams, author of “The Hitchhiker’s Guide to the Galaxy,” “Phrasing the right question is much harder than finding the right answer.”
Ultimately, it is questions – not answers – that are the driving force behind the growth of humanity’s collective intelligence and the development of a successful vaccine.
Special thanks to Johns Hopkins University & Medicine Coronavirus Resource Center and RowanSOM Family Medicine Department.
For comments/questions about this story, email editor@thewhitonline.com or tweet @TheWhitOnline.




