People who suffer from “long COVID-19,” often called long haulers, typically have experienced COVID-19 symptoms more than four weeks after their COVID-19 diagnosis, according to the Mayo Clinic.
In an article published by the American Medical Association (AMA), it’s estimated that 10% to 30% of patients experience long COVID-19, even if they experienced little to no symptoms when they were sick.
The AMA breaks down long COVID-19 into three types, starting with lingering symptoms. This is when people “do not recover completely and have ongoing symptoms because of direct cell damage from the virus,” said Dr. Sanghavi in the article.
The next type is symptoms related to chronic hospitalization. This category refers to when someone was ICU-bound for weeks, Dr. Sanghavi said. These symptoms include “cognitive brain dysfunction,” muscle weakness, and a PTSD-like syndrome.
The last type of long COVID-19 is symptoms after recovery. Dr. Sanghavi describes the final category as “symptoms that linger on are produced after the recovery because of the interplay between inflammatory markers and the immune system.”
Additionally, people may experience “acute kidney injury, which the kidneys probably won’t recover from” Dr. Sanghavi explained, resulting in possible long-term dialysis.
According to the Centers for Disease and Control Prevention (CDC), symptoms of long COVID-19 can be considered a disability.
The Mayo Clinic lists multiple signs and symptoms of COVID-19. Some of those include:
- Fatigue
- Memory, concentration, or sleep problems
- Joint, muscle, or chest pain
- Difficulty breathing
- Fast or pounding heartbeat
The article stated that some organ tissues become “severely inflamed” and patients may experience blood clots that cause heart attacks and strokes.
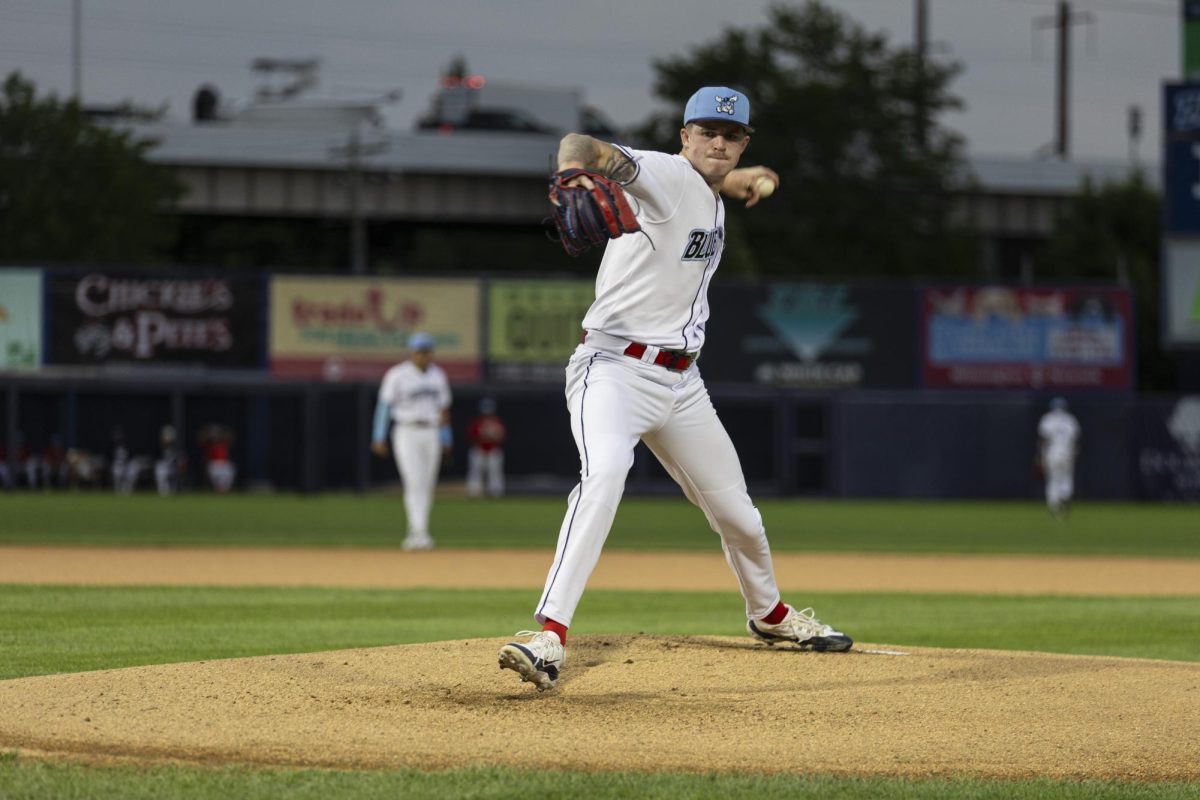
“Heart inflammation after COVID-19 is a concern, especially among young athletes returning to their sports after a mild or even asymptomatic case of the coronavirus,” read a Johns Hopkins Medicine article. “They should be screened for any signs of heart damage to ensure it is safe for them to resume activity.”
In a Rowan University YouTube video, Dr. Defendorf, an assistant professor with Rowan’s Medicine Department of Internal Medicine, was joined by Virtua cardiologist Dr. Troy Randall and Akhil Choudhary, a first-year RowanSOM Osteopathic student.
Choudhary was one of the first people in Nashville, Tennessee to get COVID-19 in March 2020 and experienced a high fever, muscle and joint pain, and brain fog for about two weeks.
“Those symptoms have since persisted,” Choudhary said. The only symptom that hasn’t continued has been the fever.
While doing schoolwork, Choudhary began to notice changes in his brain functioning.
“I was noticing gaps in memory, gaps in what I was learning. I got more stressed, my body just started to hurt more. I had a lot less energy. I found myself constantly needing to sit down during the day,” Choudhary said.
Choudhary is currently in the care of a long COVID-19 center and stressed the importance of getting vaccinated for protection against COVID-19.
Dr. Randall also contracted COVID-19 early in March 2020.
“I felt like a Mack truck hit me and I was struggling to move at times. Headaches as well,” Dr. Randall said. His symptoms gradually subsided after two weeks, but the headaches came back.
After two days, Dr. Randall went to the emergency room to discover that at some point he had a stroke.
Dr. Randall stated that he is still “functional” but still experiences brain fog.
Although more research is needed to understand how long COVID-19 affects people, it does not spare any organ, the AMA article states.
For comments/questions about this story tweet @TheWhitOnline or email [email protected].






































































































































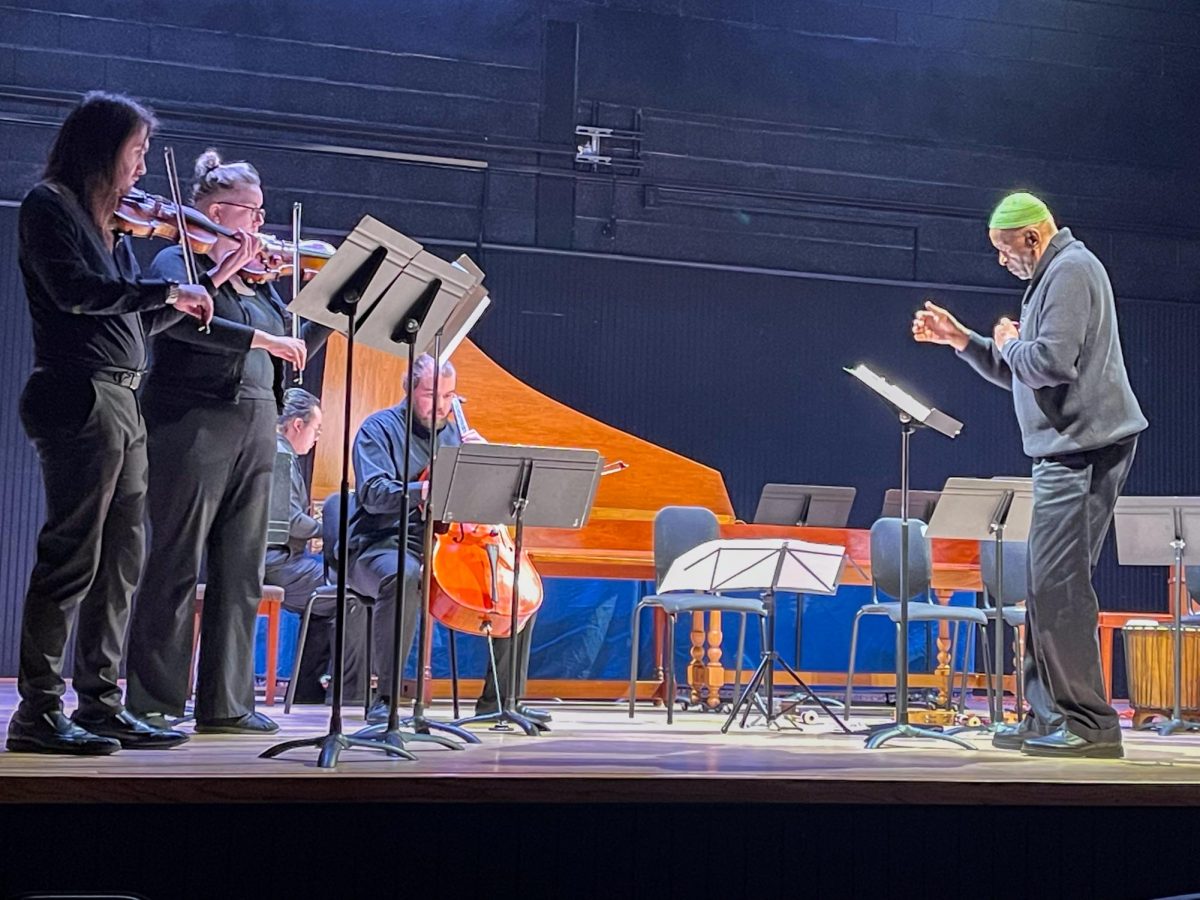
!["Working with [Dr. Lynch] is always a learning experience for me. She is a treasure,” said Thomas. - Staff Writer / Kacie Scibilia](https://thewhitonline.com/wp-content/uploads/2025/04/choir-1-1200x694.jpg)