On Oct. 14, Valerie Carabetta, Ph.D., the assistant professor of biomedical sciences at Cooper Medical School of Rowan University (CMSRU), landed a $1.8 million grant to fund research into antibiotic-resistant infections.
The Centers for Disease Control and Prevention report that every year 2.8 million or more Americans develop antibiotic-resistant infections, leading to death in more than 35,000 cases.
“If we sit back and allow this trend to continue, these bacteria will keep evolving, superbugs will continue to emerge and we will quickly return to the pre-antibiotic era, where our entire antibiotic arsenal would be useless,” Carabetta said.
Since 1928, with the discovery of penicillin by Alexander Fleming, the acknowledgment of drug-resistant bacteria has coincided with the discovery of new antibiotics. With the broad implementation of antibiotics globally, rapidly evolving bacteria have proven to grow a resistance.
“We abuse antibiotics to a certain degree. It’s not just on the side of physicians prescribing; it’s on the patients as well,” Carabetta said. “Some patients don’t finish their course of antibiotics, and then they stop taking it. Some patients self-medicate themselves, taking leftover antibiotics. A lot of this behavior leads to problems. In the agricultural industry, where they prophylactically give their animals antibiotics, we can be exposed to these bacteria that gain resistance.”
The key to any effective antibiotic is its ability to target the specific bacteria cells causing an infection and ignore our body’s natural cells. Each antibiotic class has a different strategy for doing this. Carabetta’s research looks to find new targeting methods for bacteria that haven’t evolved defenses against them. In addition, the antibiotic must be able to modify whatever chemical process it targets.
“Enzymes are proteins, which serve the function of biological catalyst. In other words, they speed up the rate of a chemical reaction inside a living cell,” Carabetta said. “Some enzymes are essential for a bacterium’s life, meaning that if they don’t function properly, the bacteria will die. Many of our current antibiotics target essential enzymes.
We need to identify some new drug targets (which is the protein that antibiotics bind to to inhibit a biological process). The histone-like proteins in Gram-positive bacteria (i.e. Bacillus anthracis, Streptococcus pneumoniae, MRSA, etc.) are essential (bacteria need to survive). The question that I am asking is, if we interfere with acetylation of these histone-like proteins, will this lead to the ultimate demise of the bacteria?”
According to Carabetta, bacteria acetylation is a modification that occurs on a protein that changes its function somehow; it’s a regulatory mechanism for bacteria. She states that the field of bacteria acetylation is a relatively young branch of science (about 12 years old), but could hold new ways for us to fight a never-ending battle against bacteria.
“To interfere with this process, we must identify a promising drug target, like an enzyme involved in adding acetyl groups or taking them off of proteins, or the histone-like proteins themselves,” she said. “My long-term goal is to understand the histone-like proteins’ functions and the enzymes that regulate them, and use this information to potentially design a new drug class.”
Carabetta’s research directly involves students and researchers alike, a facet of CMSRU’s shared location between clinical and research facilities. New members of Carabetta’s lab begin with microbiology lab basics, yet over time they are given more freedom to grow as scientists.
According to Carabetta, conducting her research at CMSRU offers unique opportunities.
“The advantage of working at a CMSRU is the close connection to Cooper University Hospital. I actually do work with some infectious disease physicians. This collaboration gives me access to actual patient isolates (meaning bacteria that are actually isolated from infected patients),” she said. “These strain collections are valuable, as it reflects resistant infections that actually arose in the community or hospital environment. So, it adds a relevant clinical dimension to any ongoing research.”
Carabetta expects her project to begin in the next two months.
For comments/questions about this story, email [email protected] or tweet @TheWhitOnline.







































































































































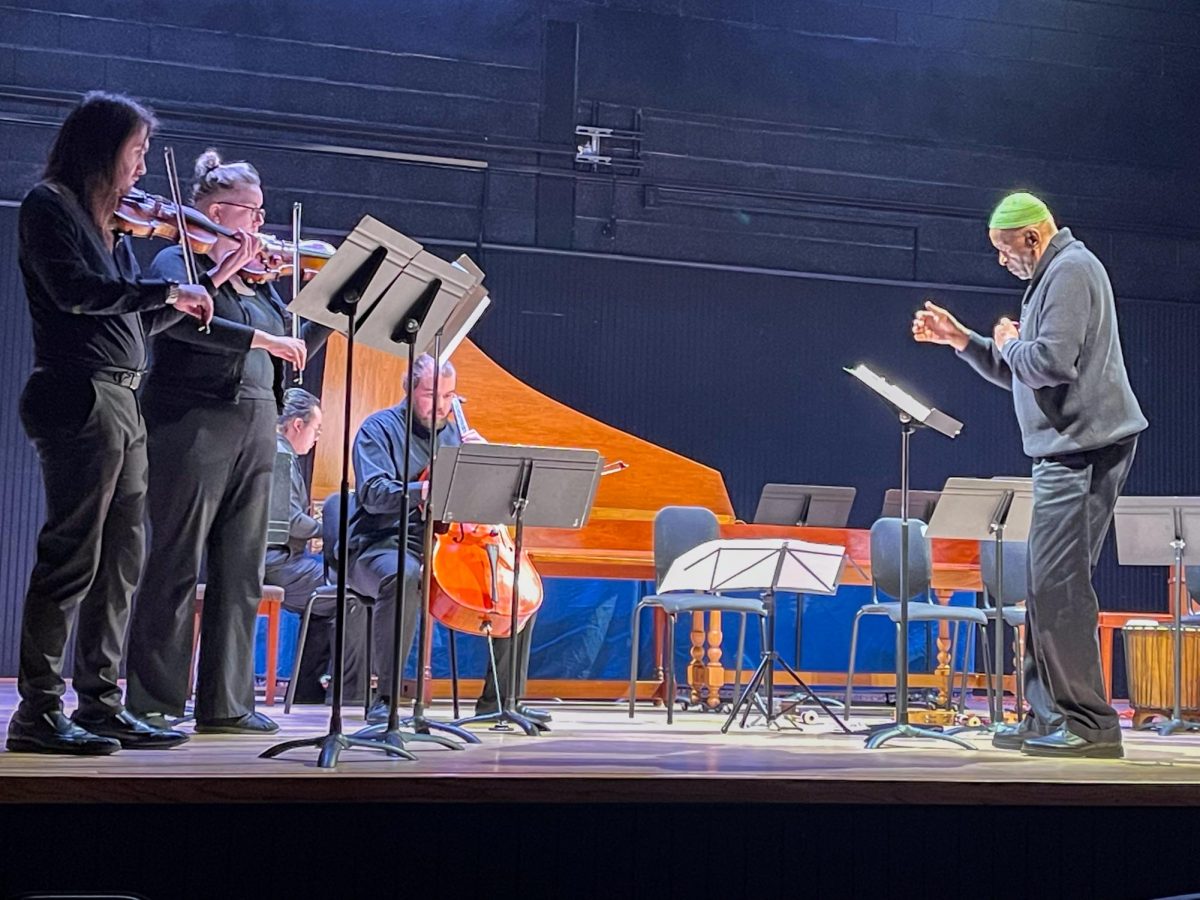
!["Working with [Dr. Lynch] is always a learning experience for me. She is a treasure,” said Thomas. - Staff Writer / Kacie Scibilia](https://thewhitonline.com/wp-content/uploads/2025/04/choir-1-1200x694.jpg)